Schizophrenia is formally classified as a mental disorder in which a person has “lost touch with reality”. Some of the symptoms of schizophrenia are categorized as hallucinatory phenomena (both audio and visual), delusions, and unusual ways of thinking. It’s considered to be an illness that is debilitating to the person as it hampers their ability to live a “normal” life.
A 2005 review in the journal Medical Hypothesis presents the history of endogenous DMT research and the proposed link between the molecule and mental disturbances including schizophrenia. A few studies in the 1970s observed greater urinary excretion of DMT amongst schizophrenic patients compared to controls. However, follow up studies found inconsistencies in this transpiration and the DMT-schizophrenia link has largely been discarded in favor of the “dopamine hypothesis”.
While much of the focus as it pertains to endogenous DMT is about measuring levels of the specific compound, it seems as though measuring the levels of monoamine oxidase (MAO) activity would provide an additional layer of insight. Monoamine oxidase is the enzyme that deaminates DMT leading to it’s breakdown and subsequent drop in measurable levels. As many of you know. the shamanic brew known as Ayahuasca contains a monoamine oxidase inhibitor (MAOI) alongside DMT in order to prevent the rapid breakdown of the psychedelic. This leads to the prolonged effects of Ayahuasca compared to inhalation or injection of DMT.
As we’ve cited in the past, a 2001 study published in the journal Life Sciences showcased the effects of increased hydroxyl radical (•OH) generation and suppression of both MAO-A and MAO-B activity. The outcome was as follows: “Results showed that the generation of •OH (hydroxyl radical) significantly reduced both MAO-A (85–53%) and MAO-B (77–39%) activities, exhibiting a linear correlation between both MAO-A and MAO-B activities and the amount of •OH produced. The reported inhibition was found to be irreversible for both MAO-A and MAO-B. Assuming the proven contribution of MAO activity to brain oxidative stress, this inhibition appears to reduce this contribution when an overproduction of •OH occurs.”
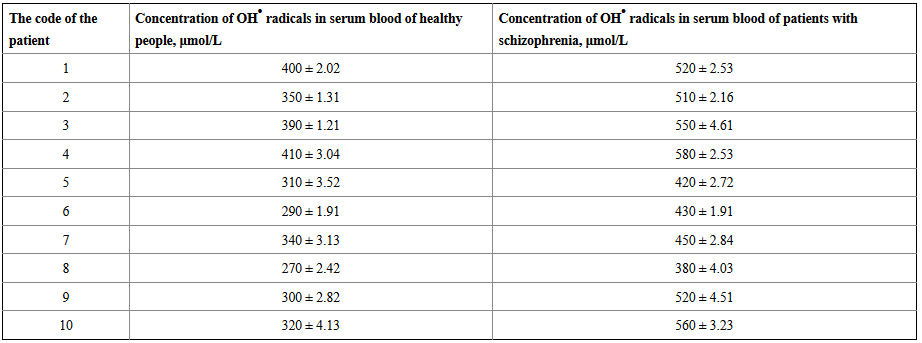
In 2011, the International Journal of Molecular Sciences published a study comparing the levels of •OH radicals of schizophrenic patients versus normal volunteers. The results found that “concentrations of •OH radicals in serum blood of healthy patients are considerably lower than in serum blood of people with pathological schizophrenia”.
(Table 1 from the 2011 study)
This data would seem to potentially revive the discussion of DMT as it pertains to schizophrenia (as well as add additional layers to the dopamine hypothesis). Suppression of monoamine oxidase activity via elevation of hydroxyl radical formation would lead to less breakdown of endogenous DMT potentially coinciding with “hallucinatory” phenomena. While we believe that there are many biochemical abnormalities relating to the symptomatology of “mental illness” outside of strictly DMT… the question is whether the DMT/monoamine oxidase activity abnormalities in schizophrenic patients is the cause or effect of the illness?
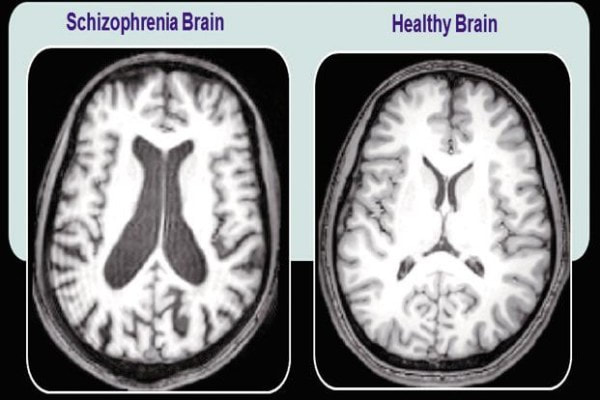
A 2016 fMRI study in the journal Psychological Medicine observed that the brains of schizophrenic patients have the ability to reorganize and regenerate. This goes against previous beliefs that brain degradation progresses linearly with no inherent repair mechanisms.
It’s important to note that neuroplastic activity has been observed from Ayahuasca ingestion in addition to neurogenesis observed from components within the Ayahuasca brew. A recent 2017 study published in Scientific Reports observed the in vitro effects of 5-MEO-DMT on human “minibrains”. It was found that proteins important for synaptic formation and maintenance were upregulated while proteins involved in inflammation, degeneration and brain lesion were downregulated. A 2015 study in ACS Chemical Neuroscience regarding the endogenous MAOI Pinoline found that it stimulated neurogensis in vitro.
These findings indicate that the upregulation of the combination of endogenous DMT(s) and MAOI’s might play key underlying factors in the regenerative capabilities of the schizophrenic brain in addition to causing some of the “hallucinatory” phenomena.
A recent 2017 study published in Molecular Psychiatry found that whole brain connectivity was detrimentally affected in schizophrenics. The two brain areas found to be affected the most were the corpus callosum (the structure that enables the two hemispheres to communicate with one another) and the frontal part of the corona radiata (a brain region key for processing information).
Another physiological correlate that has been recently identified with schizophrenia is neural inflammation (2013 Schizophrenia Bulletin, 2016 Molecular Psychiatry, 2017 International Journal of Molecular Sciences) and the upregulation of inflammatory cytokines. A cytokine is a type of signaling molecule that is excreted from the immune system. Pro-inflammatory cytokines are indicative of inflammation while anti-inflammatory cytokines serve to reduce inflammation. A 2009 study in Molecular Psychiatry found that activation of the pro-inflammatory cytokine interleukin-1β was observed in brain of schizophrenics. A 2016 study published in BMC Psychiatry found that elevated levels of pro-inflammatory cytokine IL-6 in the periphery reliably discriminated between a diagnosis of schizophrenia and normal controls. A 2017 study in the Journal of Neuroinflammation observed that another pro-inflammatory cytokine, tumor necrosis factor (TNFα) was increased in patients with schizophrenia compared to normal controls. Interestingly enough, a 2014 in vitro study observed the effects of DMT and 5-MEO-DMT in human dendritic cells via the Sigma-1 receptor and found that both DMT(s) downregulated the same pro-inflammatory cytokines (interleukin-1β, IL-6, TNFα) associated with schizophrenia. While the effects of DMT(s), pro-inflammatory cytokines, and neural inflammation when comparing in vitro studies, neural and peripheral cytokine measurements are difficult to decipher, we believe that systemic factors (likely pro-oxidant/toxin related) contribute to schizophrenia rather than simply malfunction of the DMT regulatory system. Much like the immense research that has taken place at the hands of Dr. Russell Reiter regarding melatonin and it’s multi-layered protective and regulatory abilities, DMT has also been labeled as a “biological swiss army knife” of sorts. While the negative side effects of melatonin are limited predominantly to it’s sedative qualities, similarly a negative side effect of DMT(s) could be considered “hallucinatory” phenomena (when unwanted).
This information would allude to the fact that inherent repair mechanisms exist in an attempt to combat the decreased connectivity and neural inflammation induced by chronically elevated hydroxyl radicals (and likely other inflammatory toxins). There is the potentiality that the body releases chemical compounds that attempt to stimulate activity that leads to a decrease in inflammation and increased connectivity. If increased levels of DMT(s) and suppressed MAO activity coincide with greater neurogenesis and subsequent connectivity, it doesn’t seem consistent that these factors also play a role in the neurological atrophy that coincides with mental illness.
As we touched upon in the first part of the “Gamma Wave” series, “Aha!” moments correlate with gamma waves indicating the binding of a set of neurons for the first time. This action creates a new neural pathway coinciding with greater levels of brain connectivity. In 2010, the Harvard Review of Psychiatry would publish a review of EEG data pertaining to schizophrenics finding a deficit in gamma wave amplitude. Interestingly enough, a 2015 study in JAMA Psychiatry found that spontaneous increases in gamma wave coincided with auditory hallucinations in schizophrenics. We believe that there is a definite gamma wave-DMT relationship and in schizophrenics, regional surges in DMT coincide with an attempt to retain connectivity in a degrading environment.
*It’s important to note that suppressed monoamine oxidase activity due to elevations in hydroxyl radicals isn’t a positive aspect of physiology when there is no biochemical counterbalance. Chronic exposure to oxidative stress from hydroxyl radicals can lead to neurodegeneration and subsequent “labeling” of disease. Melatonin usually plays a key biochemical counterbalance to hydroxyl radicals but in the case of schizophrenics, their melatonin levels are found to be abnormally low compared to normal controls.
We presume that DMT/Endohuasca is not the cause of schizophrenia but rather part of the complex repair mechanisms utilized by the body in an attempt to ameliorate the situation. Perhaps some of the inconclusive data in decades past regarding DMT excretion and mental illness have to do with certain patients exuding some characteristics of mental illness while not actually having the anatomical degradation associated with mental illness.
There lies the possibility that people with hyper-connected brains (such as Albert Einstein) perceive the world differently from others. Symptomatology of schizophrenia such as hearing voices, having “visions”, employing unusual thought-process methodology, and an overall disengagement of societal norms could also be found in “gifted” individuals. Many a luminary throughout history have been labeled as “crazy” at one point or another in their lifetimes. Having futuristic insights and being dissatisfied with the current status quo is hardly a reason to diagnose someone as schizophrenic. It’s important to note that without fMRI brain connectivity imaging, medical diagnosis for mental illness can be a very inexact science and utilizing “labels” does little to understand people as individuals.
In conclusion… do we believe that DMT is involved in generating some of the symptoms of schizophrenia?
Absolutely.
Do we believe that DMT is the cause of the deterioration of the brain and the subsequent diagnosis of schizophrenia?
Absolutely not.
Do we understand why the body couldn’t just repair itself without the “hallucinatory” phenomena?
No.
Do we understand hallucinatory phenomena within itself?
Not really.
The body is a complex symphony of chemical and electrical processes. The incessant quest for reductionism as it pertains to physiology is a silly endeavor that only leads to more confusion based on unnecessary unconnected discourse. It’s been noted that basic, therapeutic models involving sleep, nutrition, music, meditation, and yoga have all induced positive effects on schizophrenic patients. By contrast… environments of high stress, low quality nutrition, and insufficient sleep/sleep disturbances have all been observed to exacerbate symptoms of the disease. It would seem logical that a combination of practices that lead to optimization of one’s own basic physiology would create the necessary environment to repair damaged connectivity within the brain.
Indolethylamine N-methyltransferase (INMT) is an enzyme found in the lungs (thyroid & adrenals as well) that has been identified as being a key compound in converting Tryptamine into DMT(s). Elevated levels of INMT in schizophrenics would provide additional support for the DMT-schizophrenia theory. A 1972 study in the journal Life Sciences was published comparing the blood levels of INMT of schizophrenic volunteers (acute and chronic) versus normal controls. The results were as follows: N-methyltraneferase activity is not detectable in normal controls, but is present at detectable levels in both chronic and acute schizophrenics. This adds credence to our postulation that DMT(s) are not normally measurable in the periphery (blood) due to intact integrity of the blood brain barrier (and possibly gut-barrier). Patients with schizophrenia have been observed to exude increased permeability of the blood-brain barrier as well as gut-barrier permeability possibly coinciding with neural inflammation and leakage of epithelial-barrier produced biochemicals (such as DMT) into the periphery.
*A 2010 study published in Neuro Endocrinology Letters measured bufotenin (5-HO-DMT) levels in the urine of patients with schizophrenia and autism compared to control volunteers. It was observed that the urine of schizophrenic subjects contained nearly 300% more bufotenin than the controls. This is an interesting and important study as it utilizes a more modern assay/equipment than what was utilized in the 1970’s albeit the sample size was relatively small. While not schizophrenic specific, 2 studies found that tribulin (an endogenously produced MAOI) was upregulated in the brain following stress in animals as well as exuded increased urinary output in agitated patients with post traumatic stress disorder.
(There are numerous studies showcasing a definitive relationship between suppressed monoamine oxidase activity and schizophrenia. However, most of the studies pertain directly to MAO-B suppression in the platelets rather than MAO-A (There are 2 types of monoamine oxidases in the body). Nevertheless, it seems as though suppression or distinct changes in MAO-A activity is potentially taking place as it coincides with the dopamine hypothesis (excessive activity of certain dopaminergic circuits) of schizophrenia. Numerous studies have showcased genetic changes in MAO-A within schizophrenics. This could allude to the notion that the deamination process could be altered affecting the rate in which DMT (as well as other monoamine neurotransmitters) is broken down. Wild speculations indeed…)
DMT Quest is a non-profit 501(c)3 dedicated to raising awareness and funds for endogenous DMT Research. This specific field of psychedelic research has been underfunded for many decades now. It’s time to take our understanding of human physiology, abilities, and perception to the next level. E-mail me at jchavez@dmtquest.org with any comments or questions. You can also follow us on Facebook, Instagram, or Twitter.